The rapid emergence of severe avian influenza cases in humans has raised alarms across the United States, with the most concerning instance being an elderly patient in Louisiana who is currently in critical condition due to the H5N1 virus. This case signifies not just a local health crisis but reflects a broader global fear of a potential pandemic that could arise from avian influenza. The implications of this situation are vast, from public health to agricultural policies, necessitating a thorough examination of facts, responses, and future considerations.
As of now, there are 61 confirmed cases of avian influenza within the United States, including this severe case in Louisiana. The Centers for Disease Control and Prevention (CDC) has noted that the afflicted patient had contact with sick and deceased birds from backyard flocks. Historically, significant human infections have prompted global health concerns due to the severity associated with H5N1 infections. This is not merely a statistical anomaly; the danger of the virus has been validated over the last two decades, as it has exhibited a roughly 50% fatality rate in documented human cases internationally. With this critical Louisiana patient now hospitalized, it underscores increased vigilance required from health officials and the public alike.
California’s decision to declare a state of emergency appears pragmatic in this context. Governor Newsom highlighted the importance of resources and flexibility for government agencies to ensure a rapid response to the outbreak. Such preemptive measures are crucial as they can mitigate the spread of the virus and protect vulnerable populations, especially those with underlying health conditions.
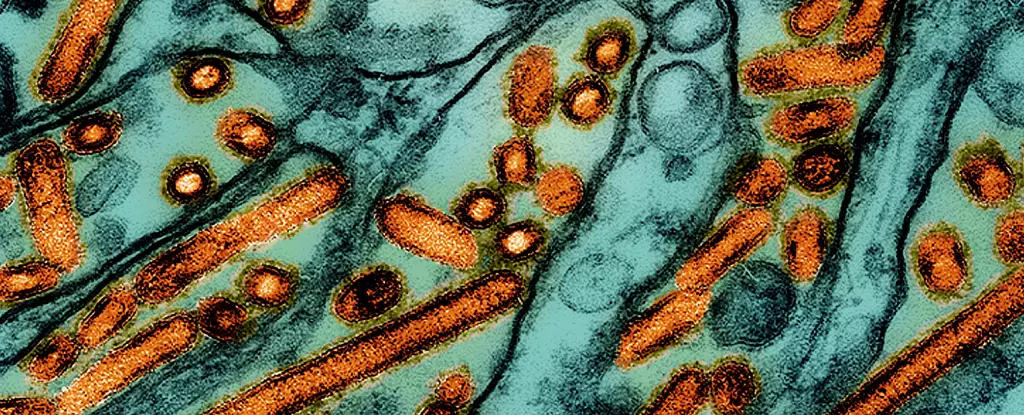
A deep understanding of the H5N1 virus’s genetic makeup is essential to grasp its potential threat fully. In Louisiana, genetic sequencing revealed that the virus corresponds to the D1.1 genotype. This strain is currently spreading among wild birds and poultry within the United States, similar to strains found in other human cases, including one documented in British Columbia. The distinctions between genotypes indicate differing transmission patterns and virulence; for instance, the B3.13 genotype has been associated with milder cases in humans.
The implication here is profound: as certain genotypes demonstrate more significant potential for severe disease, health officials must continually adapt their monitoring strategies. Increasing surveillance is paramount, as many cases remain without an identifiable animal source, raising questions regarding reporting accuracy and the potential for asymptomatic human transmission.
While some health experts express cautious optimism, others urge for greater alarm. Rebecca Christofferson from Louisiana State University articulated a careful approach, suggesting that panic is unwarranted, yet increased vigilance is non-negotiable. Contrast this with remarks from Meg Schaeffer from the SAS Institute, who articulates a mounting concern that “avian flu is knocking on our door” and could potentially trigger a new pandemic. This divergence in professional opinion highlights the ongoing debate among researchers and public health officials regarding the appropriate level of response in light of potential risks.
The stockpiling of vaccines by the US government serves as a strategic move, preparing for the inevitable possibility of human transmission. Furthermore, research into an experimental mRNA vaccine has demonstrated promising results in preclinical trials, notably protecting ferrets from serious implications of the virus. Should this be successfully translated to human applications, it could significantly alter the trajectory of avian influenza outbreaks.
One pivotal aspect of mitigating this outbreak involves addressing agricultural health and the potential vectors of transmission. The connection between raw milk and the risk of virus spread cannot be overlooked, prompting the US Department of Agriculture to implement more stringent reporting requirements regarding raw milk testing for avian influenza. This decision indicates heightened awareness of the interconnectedness of animal health, food safety, and human health.
Moving forward, the challenge lies not just in containment but in fostering a comprehensive public health strategy that prioritizes surveillance, rapid response, and extensive research into effective vaccines. Public health messaging is equally critical; educating communities about the risks and promoting preventive practices will play a vital role in curbing potential outbreaks.
The emergence of severe avian influenza cases in humans necessitates a robust, multidisciplinary response from public health authorities, industry stakeholders, and the global community. As we navigate the complexities of this evolving health crisis, adaptive strategies and preventative measures will be key to ensuring public safety and averting a possible pandemic. The time for detailed scrutiny and bold action is now, as we work to safeguard the health of communities nationwide.

Leave a Reply