In a significant development for the pharmaceutical and healthcare sectors, Medicare has confirmed that Eli Lilly’s weight loss drug Zepbound will now be covered for patients suffering from obstructive sleep apnea (OSA). This decision not only marks a pivotal moment for those impacted by obesity and sleep-related breathing disorders but also illuminates the broader complexities of Medicare’s drug coverage policies.
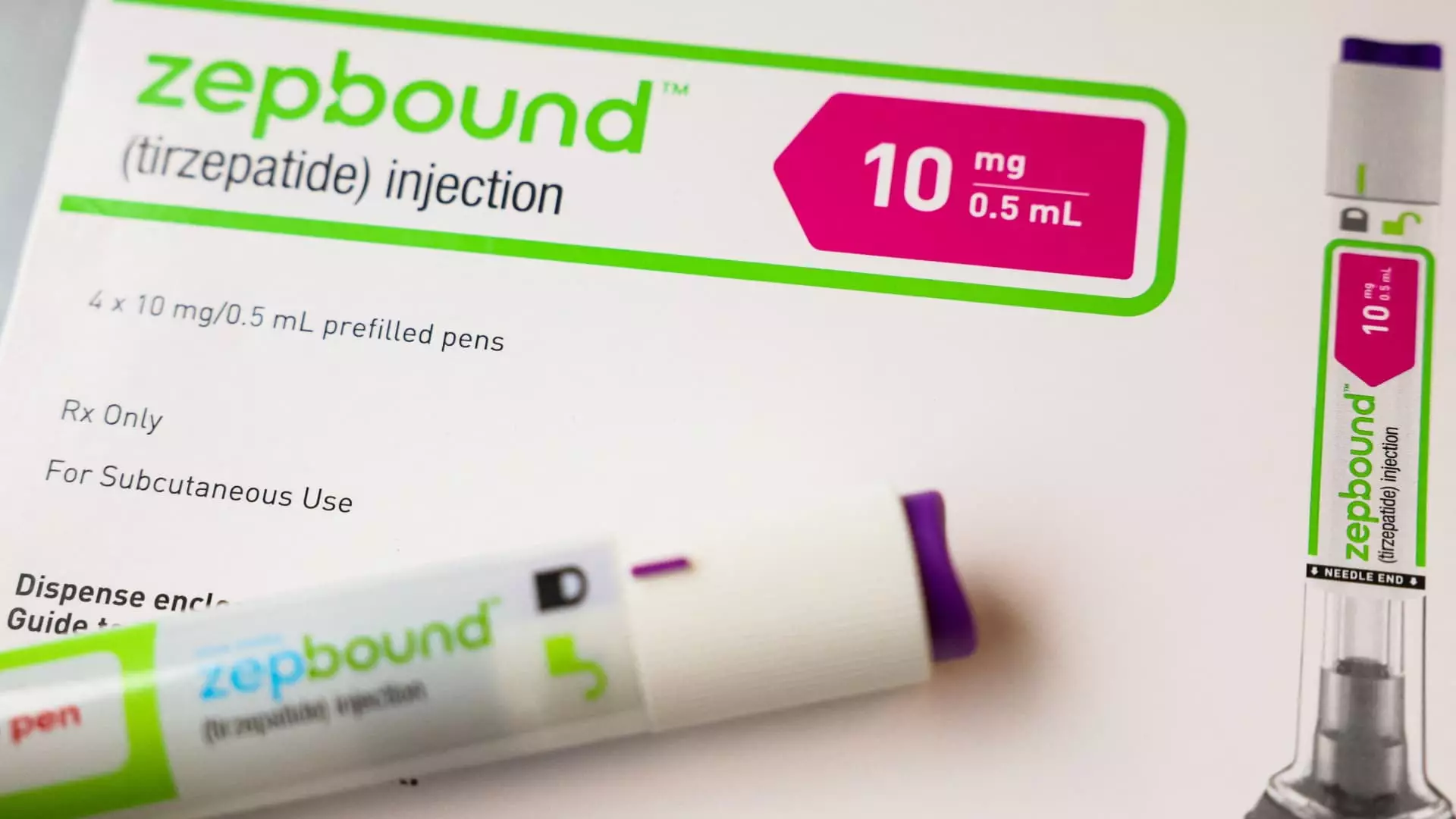
Zepbound has gained recognition as a promising treatment in the fight against obesity, particularly for individuals also battling obstructive sleep apnea. Despite its impressive efficacy, the drug’s near $1,000 price tag—before insurance—inhibits access for many individuals. Yet, over the past year, demand for Zepbound has surged remarkably, demonstrating a growing acknowledgment of obesity as a serious medical condition that warrants effective interventions.
This juxtaposition of demand and cost brings forth an essential discussion about the role of insurance companies, particularly Medicare, in making these lifesaving medications accessible. The Centers for Medicare & Medicaid Services (CMS) have stated that Zepbound will be evaluated under existing Medicare Part D and Medicaid coverage guidelines, which require that the drug be utilized for an FDA-approved indication beyond mere weight loss. Such stipulations could complicate the accessibility of Zepbound, requiring patients to navigate a process laden with bureaucratic hurdles, such as prior authorization—that is, obtaining insurer approval before a prescription can be filled.
A crucial facet of the coverage landscape is the need for pharmaceutical companies to ensure that their products align with regulatory expectations. As highlighted by a CMS spokesperson, for a drug to be covered under Medicare Part D, it must be prescribed not only for weight management but for additional medically accepted uses recognized by the FDA. In this context, Eli Lilly is navigating a sensitive environment where understanding these nuances is vital for both the company and the patients it seeks to help.
Zepbound’s recent FDA clearance for OSA underscores its significance for an estimated 20 million patients grappling with this condition. The timing of this approval could not be more critical; as awareness of OSA grows, so does the demand for effective treatments. However, the divergent paths for state Medicaid programs present another layer of complexity, making clear that coverage can vary widely based on specific conditions for which a drug is prescribed and the agreements made between manufacturers and state governments.
Amid this backdrop, the Biden administration’s proposal in November aimed at expanding coverage for weight loss drugs under Medicare and Medicaid could reshape the landscape of obesity treatment. Should this rule come to fruition, it may not only improve access to effective treatments for millions of Americans battling obesity but also significantly impact healthcare costs—an estimated $35 billion over ten years. Whether this proposal will survive the political landscape and garner support in light of changing administrations remains unclear.
The dialogue surrounding obesity treatment, notably through drugs like Zepbound and competitors such as Novo Nordisk’s Wegovy, can be reflective of broader societal attitudes toward obesity. While traditionally stigmatized, there’s a growing recognition within policy circles that obesity is a medical issue requiring comprehensive treatment approaches, including pharmacological interventions. This shift could further normalize discussions about obesity management and treatment options in both public and private healthcare settings.
As healthcare professionals, policymakers, and advocates work together to address the challenges presented by obesity and obstructive sleep apnea, it is imperative that they remain aware of the implications of these critical developments. For Zepbound, being recognized as a part of the Medicare drug benefit program is a step forward—but it is only part of a larger journey toward comprehensive care.
The healthcare community must continue to advocate for policies that ensure equitable access to treatments and maintain ongoing dialogue about the value of addressing obesity as a systemic health issue. Only then can we hope to create a future where effective treatments like Zepbound are accessible to all who need them, transforming lives and health outcomes on a wide scale.

Leave a Reply