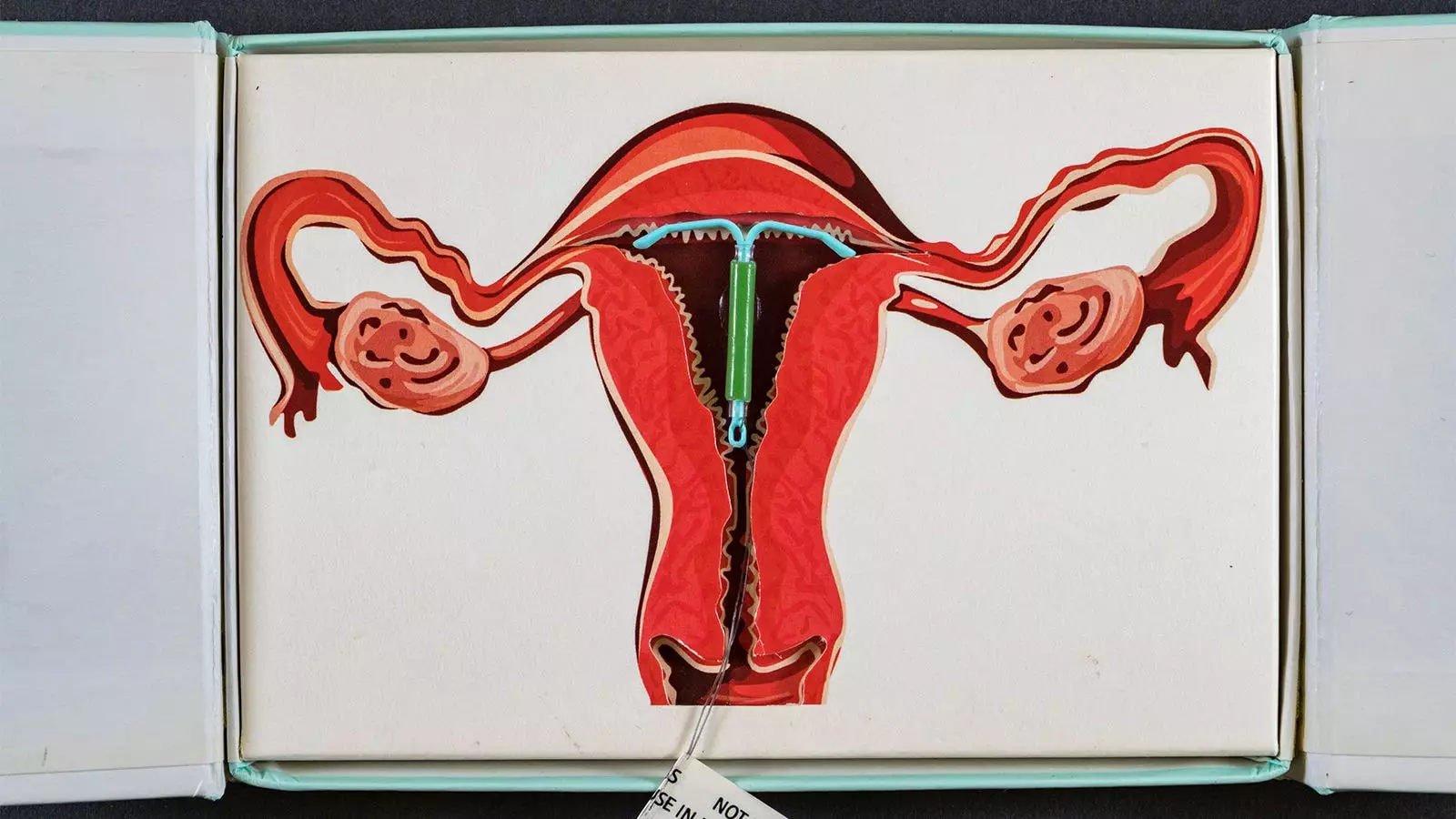
The discourse surrounding hormonal contraceptives, particularly intrauterine devices (IUDs) and their potential association with breast cancer, has become increasingly pertinent in recent years. A significant body of research, including a recent study from Denmark, sheds light on the elevated risks associated with the hormonal levonorgestrel-releasing IUD (LNG-IUS). This article seeks to dissect the findings of the study, contrast them with existing literature, and highlight the implications these findings hold for women considering hormonal contraceptive options.
Conducted over nearly seven years, the Danish registry study revealed alarming statistics: women under 50 years utilizing LNG-IUS experienced a 40% greater likelihood of being diagnosed with breast cancer compared to their counterparts who abstained from hormonal contraceptives. With a focus on the duration of use, the data indicated that the risk escalated drastically—showing an 80% increase in those who used the device for a span of 10 to 15 years. While the findings reported an elevated incidence—ranging from 14 to 71 additional cases of breast cancer per 10,000 LNG-IUS users—the researchers noted that some of the statistical trends lacked significance.
The meticulous nature of this study is noteworthy. By leveraging national healthcare registries and focusing on a specific cohort of first-time users aged 15 to 49 from 2000 to 2019, the researchers managed to offer a robust comparison between users and non-users of hormonal contraception. The matching of over 78,000 representatives from both groups further strengthens the integrity of the findings.
Understanding Hazard Ratios
The concept of hazard ratios (HR) plays a crucial role in the interpretation of the study outcomes. The HR of 1.4 for LNG-IUS users indicates a 40% higher breast cancer risk relative to non-users. More incisively, the analysis breaks down the hazard ratios further into time categories: 1.3 for 0-5 years of use, 1.4 for >5-10 years, and a stark 1.8 for >10-15 years, pointing to a clear correlation between prolonged use and increased risk.
However, the study authors also issued a cautionary note regarding the statistical significance of these trends. With a P-value of 0.15 for the trend analysis, the assertion of a direct causal link requires further inquiry, as this suggests the results might be influenced by variables that were not measured or considered.
Given the rising adoption of LNG-IUS, particularly among younger women who face various reproductive health challenges, the implications of these findings are profound. The duality of benefitting from reliable contraceptive measures while bearing increased health risks leads to a critical need for increased transparency and informed decision-making regarding contraception options.
The authors of the study emphasize the necessity for healthcare providers to discuss risks alongside the benefits of LNG-IUS. Considering the potential long-term reliance on these devices as a form of contraception, this becomes even more crucial. Past studies have provided insights into the risks associated with short-term LNG-IUS use; however, the current findings cast a more extensive net, thereby prompting a reevaluation of the advisability of such contraceptive methods, particularly among those with a genetic predisposition to breast cancer, such as BRCA1 carriers.
The emerging data regarding the asymmetrical relationship between LNG-IUS usage and breast cancer risk compels a call for further research. Women deserve complete and comprehensive information to navigate their health choices effectively. As the medical community continues to unravel the complexities of hormonal contraceptives, it must strive to strike a balance between advocating for effective reproductive autonomy and safeguarding against potential long-term health risks.
While the Danish registry study adds to the evolving narrative of hormonal contraceptives’ implications for women’s health, it underscores the importance of continued investigation into the long-term effects of these methods and the imperative for informed discussions between healthcare providers and patients.

Leave a Reply