The alarming rise of obesity among children and adolescents presents a multifaceted challenge to healthcare practitioners, educators, and families alike. This issue is particularly pressing among younger age groups, where the consequences of severe obesity can manifest through a myriad of health complications. As advancements in obesity treatment continue to evolve, easing the burden on affected children and their families demands thorough scrutiny of both pharmacological and lifestyle interventions.
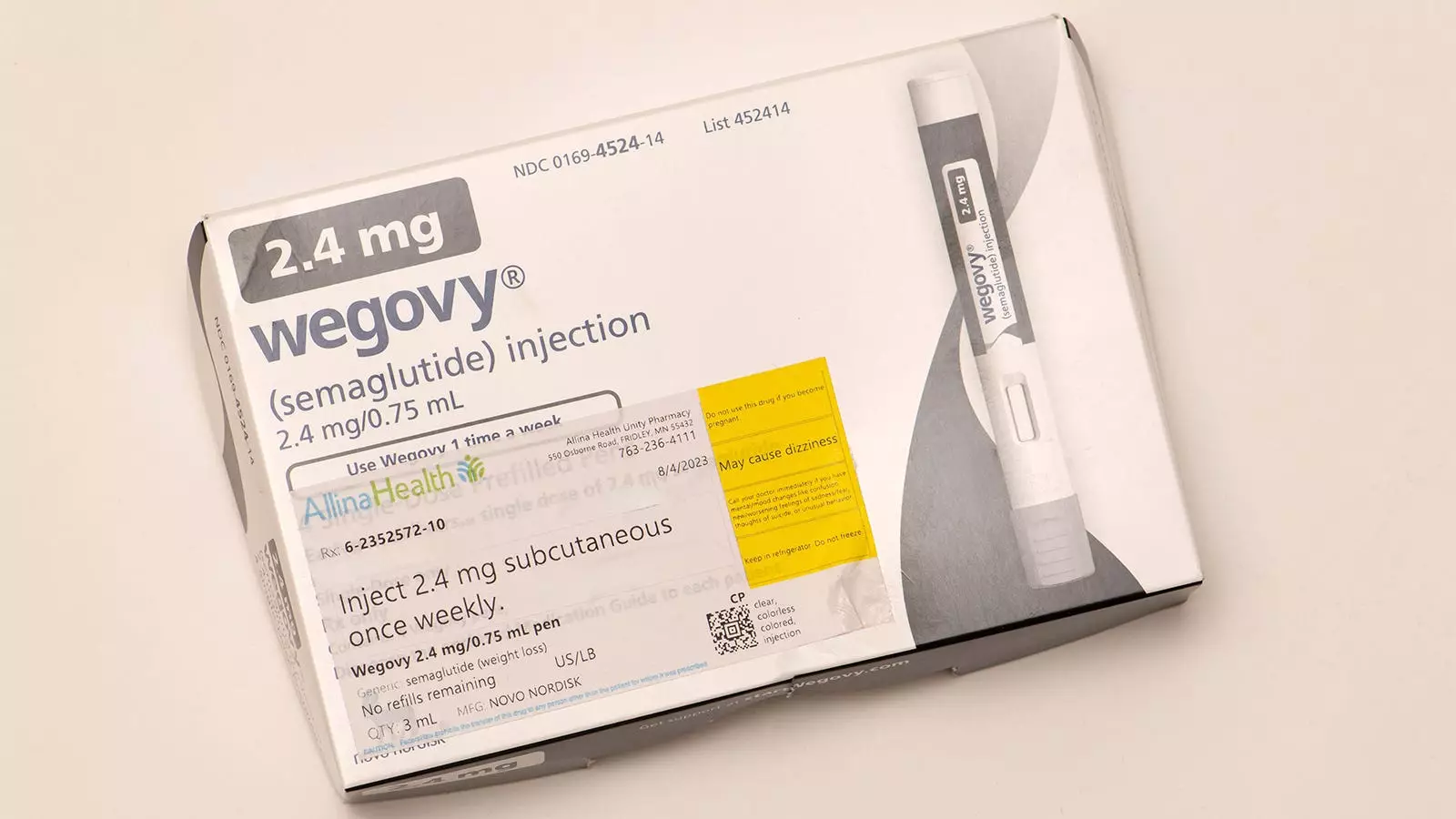
As a specialist in pediatric obesity medicine, I have been privy to the significant impact that GLP-1 receptor agonists, particularly semaglutide (marketed as Wegovy), have made in managing obesity among adolescents. It is noteworthy that when paired with an intensive health behavior modification program, these medications have shown considerable benefits in improving various health risk factors. Young patients have demonstrated enhanced tolerance for physical activities, better sleep quality, a more positive body image, and increased self-confidence.
The conversation, however, shifts significantly when we consider the younger population, particularly those under 12 years old. Here, despite the presence of severe obesity and its associated health risks—ranging from prediabetes to bullying—available pharmacological treatments are alarmingly scarce. This ongoing predicament might see a shift soon as the FDA deliberates the potential approval of liraglutide for treating severe obesity in children aged 6 to 12. Recent findings published in the New England Journal of Medicine have added a sense of optimism, showcasing evidence of liraglutide’s safety and efficacy alongside structured lifestyle interventions.
The randomized trial involving 82 children across multiple centers indicates promising outcomes regarding the efficacy of liraglutide. Children receiving a regimen of 3 mg of the drug, coupled with behavioral interventions, experienced a notable reduction in BMI—5.8% compared to the 1.6% increase observed in the placebo group over a 56-week period. However, it is essential to interpret these results with caution. While the medication demonstrated a positive trend in reducing BMI, there were no statistically significant improvements in critical metabolic markers like blood pressure or hemoglobin A1c.
Moreover, the side effect profile of liraglutide prompts reflection. A substantial 80% of children treated with the drug reported gastrointestinal side effects, albeit most cases were classified as mild to moderate. The implications of such side effects, especially considering the nuanced needs of this vulnerable demographic, cannot be overlooked.
Analyzing Risks and Benefits in Context
The decision to prescribe pharmacological interventions to children necessitates a careful balance of risks and benefits. The American Academy of Pediatrics suggests that weight loss medication can be offered to children ages 8 to 11, provided the benefits outweigh the risks. However, the necessity for FDA approval looms large, underlining a significant barrier before liraglutide can become a viable option in clinical practice for young children.
When weighing the pros and cons of introducing medications like liraglutide, several factors come into play. On the positive side, there may be a modest reduction in BMI and potential improvements in metabolic and psychosocial risk factors. Unfortunately, critical unknowns loom around long-term safety and efficacy, particularly concerning growth and the eventual impact on adult height.
Equally concerning are the long-term outcomes post-medication. Data from the trial indicate that nearly all weight lost during treatment was regained once the medication was discontinued. This highlights a fundamental issue in obesity management: the sustainability of weight loss and the behaviors that accompany pharmacological interventions.
While the potential FDA approval of liraglutide presents new avenues for treating severe obesity in children aged 6 to 12, a comprehensive evaluation of its risks and benefits is critical. It is imperative that we recognize that severe obesity is a complex disease necessitating personalized treatment strategies. The introduction of medications must be accompanied by a robust, multi-disciplinary approach that prioritizes intense lifestyle interventions.
As researchers continue to explore effective treatments for pediatric obesity, the health and well-being of affected children must remain at the forefront of clinical decision-making. My hope is that with careful consideration and ongoing research, we may soon have more effective, safer strategies for helping these children navigate their unique challenges—in an effort to ensure they don’t fall behind in the quest for a healthier future.

Leave a Reply