The ongoing dispute within the NHS exposes a fundamental flaw in how we perceive and address healthcare challenges. The narrative often simplifies complex issues—blaming either the staff’s greed or the government’s negligence—without considering the deeper systemic failures. Labeling the resident doctors’ demands as solely rooted in greed dismisses a broader context: years of stagnating wages amid rising living costs, burnout from relentless work hours, and a sense of undervaluation that has festered over nearly two decades. The government’s stance that a 29% pay increase was already granted seems superficial when viewed through the lens of the cost of living crisis and the actual erosion of real income these professionals have suffered.
This is not merely a pay dispute; it is an indictment of a healthcare system that has lost its capacity for fairness and sustainability. To judge these doctors as avaricious misses the point that their struggle serves as a mirror reflecting the NHS’s failure to respect and adequately compensate those who form its backbone. Simply put, the crisis is rooted in neglect, not greed. And by focusing so heavily on monetary figures, policymakers ignore the human consequences of their policies, which have driven many skilled professionals to the brink of burnout or out of the profession altogether.
Political Posturing and Public Perception
The ongoing standoff reveals a dangerous game of political blame-shifting. The government, represented here by Health Secretary Wes Streeting, seeks to control the narrative by emphasizing “local decision-making” and prioritizing urgent, critical care. While such decentralization sounds pragmatic in theory, it risks turning into a dangerous abdication of national responsibility. It’s a convenient way to dodge the uncomfortable truth that the NHS, underfunded and overburdened, cannot simply rely on local trusts to patch its broken parts.
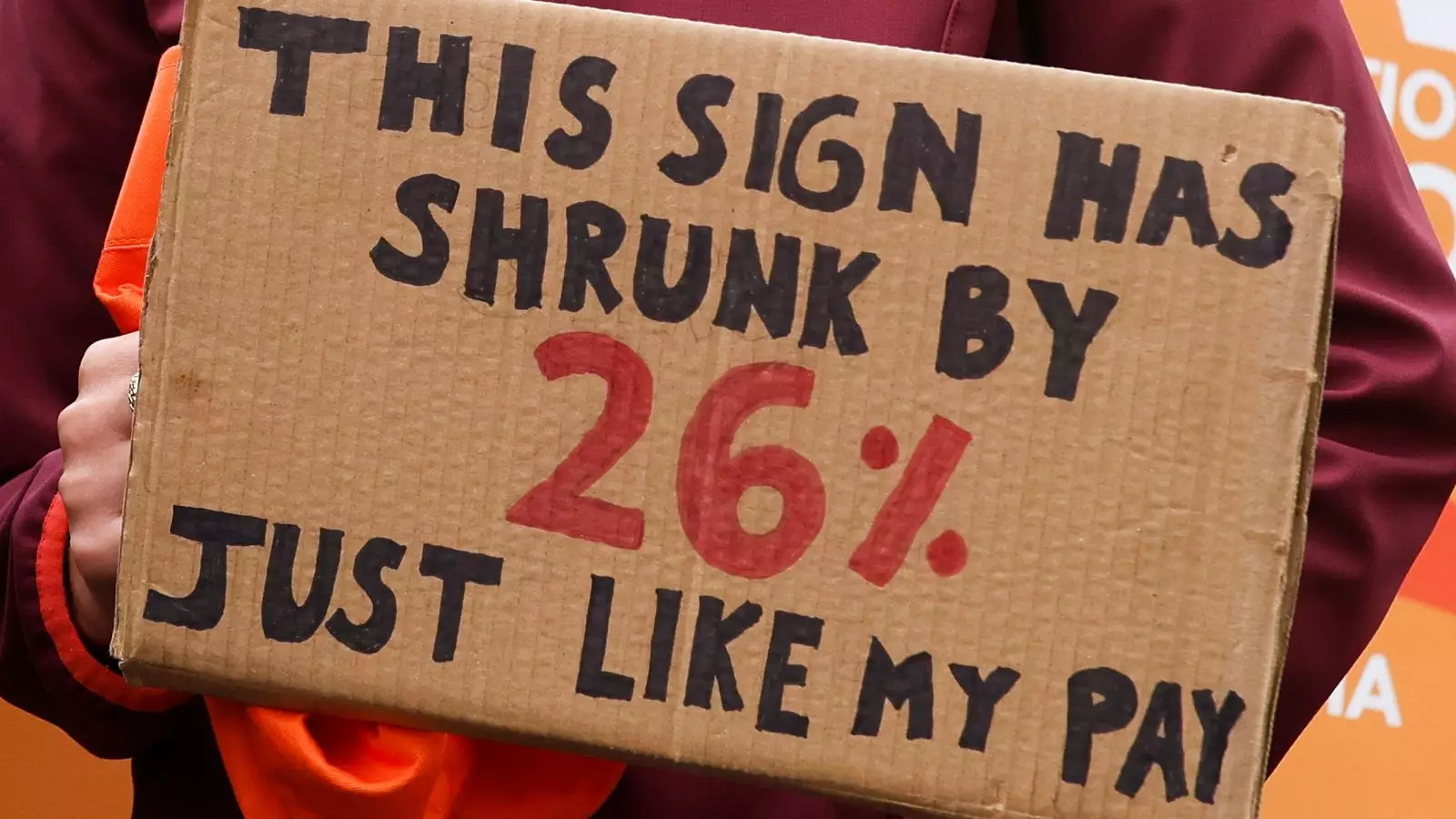
Meanwhile, the unions, particularly the BMA, frame their demands as long-overdue justice—a rightful correction for years of underpayment. But their rhetoric feeds into a culture of entitlement that can alienate the public, especially when figures like the 26% pay restoration are presented without sufficient context. Public support wanes when strikes threaten to jeopardize essential services, and governments seize this opportunity to paint doctors as selfish or irresponsible. This polarizing narrative deepens societal divides and hampers meaningful dialogue. It’s a disturbingly simplistic binary that ignores the nuanced realities faced by both sides.
Systemic Failures and the Future of NHS Reform
The core issue remains: the NHS’s structural fragility. Ambitious reform plans and long-term visions become meaningless if the workforce feels alienated and undervalued. Without addressing the root causes—wage stagnation, excessive workloads, administrative overreach—the NHS risks a continued drain of talent and public confidence. Promoting local decision-making might seem a way to empower trusts, but unless underpinned by adequate funding and a commitment to fair treatment, it is merely a Band-Aid for a gaping wound.
The real question is how to forge a sustainable path forward that recognizes the essential role of health workers as partners, not adversaries. Chronic underfunding and politicized negotiations have left the NHS vulnerable, and superficial solutions will only exacerbate this rift. If policymakers continue to ignore the systemic flaws—namely, the failure to modernize and adequately care for those who care for us—the cycle of strikes and setbacks will persist, endangering the very foundation of our healthcare system.
The Human Cost of Political Standoff
Beyond the headlines and political language lies a profound human tragedy. Patients waiting for treatment, elderly individuals facing postponed appointments, and families impacted by cancelled procedures are the silent victims of this discord. The NHS was built on a principle of universal care, but sustained political wrangling is eroding that ideal. When healthcare becomes collateral damage in a battle of narratives—whether centered on fairness, funding, or blame—the integrity of the system is compromised.
The current approach, favoring local discretion and incremental decisions, risks fragmenting a once-unified national service. Without decisive, equitable action rooted in real investment and respect for healthcare workers, the NHS’s foundational promise of care for all will fade into a distant memory. It is high time for a frank, reform-minded conversation that centers on human dignity, fair compensation, and the collective responsibility we owe to those who dedicate their lives to public health. Anything less threatens to propel us further into chaos and disillusionment.

Leave a Reply