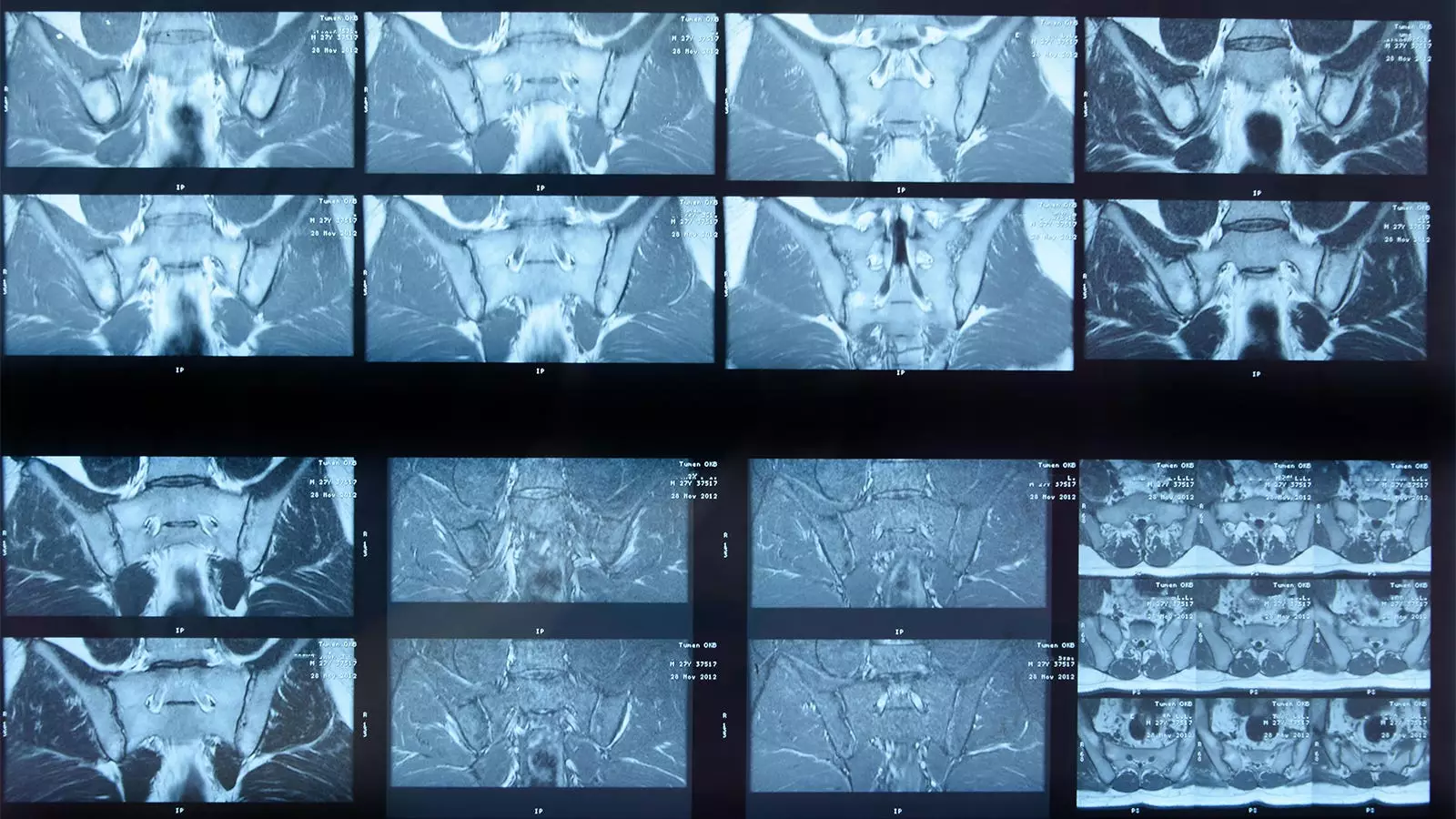
Artificial intelligence (AI) is making significant strides in various domains, and the field of medical imaging is no exception. One prime area of focus is the integration of deep learning algorithms in analyzing MRI scans, particularly for diseases like axial spondyloarthritis (axSpA). A recent study led by Joeri Nicolaes, PhD, alongside colleagues from UCB Pharma, has shed light on the effectiveness of a newly developed AI algorithm in detecting sacroiliac joint (SIJ) inflammation among axSpA patients. While the findings demonstrate a commendable performance, they also raise critical discussions around the current limitations and future potential of AI in this essential medical arena.
The AI algorithm was rigorously tested against a set of MRI scans sourced from two extensive clinical trials, RAPID-axSpA and C-OPTIMISE, involving a total of 731 patient images. Strikingly, the algorithm demonstrated acceptable concordance with expert human readers through its analysis, achieving agreement on 543 out of the 731 images. In specific terms, both the AI system and human experts identified inflammation in 304 images and correctly recognized no inflammation in an additional 239 instances.
However, the study does not end on a high note; discrepancies were encountered in 132 cases, where experts detected inflammation that the algorithm failed to recognize. Meanwhile, in 56 images, the AI inaccurately flagged inflammation that the experts deemed non-existent. The researchers, while acknowledging the AI’s limitations, emphasized that such discrepancies are not uncommon given the evolving nature of medical imaging and interpretation.
A closer examination of the algorithm’s statistical performance reveals a nuanced picture. Absolute agreement stood at 74%, with sensitivity at 70% and specificity at 81%. The positive predictive value (PPV) reached 84%, while the negative predictive value (NPV) was noted at 64%. Furthermore, the Cohen’s kappa statistic—often used to quantify inter-rater reliability—was calculated at 0.49. While these values indicate an overall acceptable level of performance, the researchers were quick to highlight certain contextual factors that could have impacted these outcomes.
Crucially, the definition of SIJ inflammation utilized in the study was perceived as conservative, suggesting that expert readers might have employed supplementary clinical data when reaching their conclusions. This acknowledgment calls into question the reliability of baseline assumptions underpinning the study, indicating a need for recalibrating expectations regarding AI algorithms in intricate clinical scenarios.
One of the primary appeals of AI algorithms lies in their ability to produce reproducible results. Unlike human readers, whose interpretations can vary due to personal biases or capabilities, AI systems can deliver consistent assessments of MRI scans. This aspect could be particularly beneficial in settings where trained expert readers may be scarce. As Nicolaes and his colleagues noted, the qualifications of the expert panel in this study might far exceed those of general radiologists, reinforcing the notion that machine learning could serve as a valuable support tool in less specialized environments.
However, the absence of contextual elements like C-reactive protein (CRP) levels or HLA-B27 positivity in the algorithm’s processing leaves significant room for improvement. The integration of such factors may enhance the algorithm’s precision and reliability, ultimately optimizing its utility in clinical practice.
Despite the study’s promising developments, notable challenges persist. One significant limitation was that a substantial number of scans could not be processed due to image size and slice count restrictions inherent to the algorithm’s design. This limitation poses questions about the algorithm’s practicality in real-world applications where variability in imaging methodology is commonplace.
Additionally, the researchers recognized the evolving standards in SIJ inflammation classification since the algorithm’s inception, underscoring the need for it to undergo further updates to maintain clinical relevance. Moreover, the algorithm’s current inability to detect structural damage—a critical factor for treatment planning—needs to be addressed.
The progression of deep learning algorithms in the detection of conditions such as axSpA is undeniably valuable. The research by Nicolaes and colleagues marks a pivotal step towards incorporating AI into routine clinical assessments of MRI scans. However, the study’s findings, coupled with its limitations, serve as a reminder of the intricate nature of medical diagnostics. Continuous evolution, rigorous testing, and adaptability to clinical practice standards will be vital elements in the future effectiveness and acceptance of AI technologies in medical imaging. As the landscape of diagnostics transforms, the collaboration between human expertise and machine learning will ultimately dictate the degree to which these innovations enhance patient care.

Leave a Reply