Selective serotonin reuptake inhibitors (SSRIs) have become a staple in the treatment regimen for mood disorders, particularly anxiety and depression. Millions of patients rely on these medications, yet there is an ongoing debate about their long-term effectiveness and how they exert their effects in the brain. This uncertainty is heightened by the complexities of mental health, where cognitive functions such as memory and reasoning can be profoundly affected by both the disorder and the treatment itself. Recent research from Copenhagen University, spearheaded by psychologist Vibeke Dam, aims to investigate this intricate relationship between SSRIs, cognitive function, and mood.
In a study involving 90 patients diagnosed with moderate to severe depression, researchers sought to catalog the cognitive effects of the SSRI escitalopram over an eight-week treatment period. The study was multi-faceted, employing brain scans, cognitive tests, and mood evaluations before and after the treatment to build a comprehensive picture. At the outset, the participants underwent thorough assessments to establish a baseline. By the end of the eight weeks, 40 subjects had repeat brain scans, and all participants completed a final round of cognitive and mood assessments at 12 weeks.
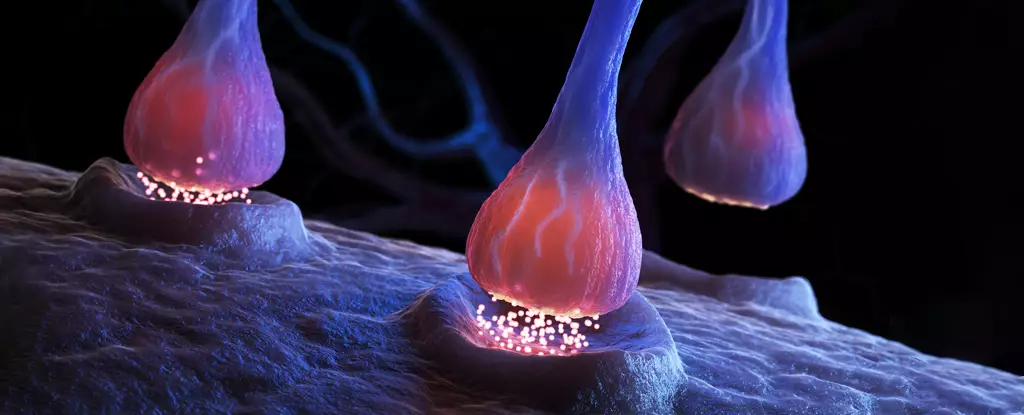
Notably, a profound reduction—approximately 10 percent—was observed in the cell receptors targeted by SSRIs between the initial and final assessments. More strikingly, patients displayed significant enhancements in cognitive tasks, particularly in word recall abilities. Interestingly, the most notable improvements in verbal memory were linked to minimal changes in the serotonin receptor known as 5-HT4. These findings suggest a potential mechanism where the remaining serotonin receptors might become more efficient due to increased serotonin levels in the synapses, even when receptor binding decreased.
Vibeke Dam hypothesized that this specific receptor, 5-HT4, may play an essential role in cognitive enhancement associated with SSRIs. However, the lack of a correlation between the changes in receptor binding and mood improvements raises pivotal questions. While cognitive function benefits are evident, the mood changes appear inconsequential in parallel, pointing to the complexity of biological mechanisms behind antidepressant efficacy.
This disparity further complicates the narrative around SSRIs. The study hints at possible implications for developing targeted treatments that could alleviate cognitive deficits in depression, independent of improvements in mood. This direction is particularly intriguing, as cognitive deficits often persist even in patients who experience mood stabilization.
Despite the insights offered by this study, researchers face ethical challenges, notably the inability to include a placebo group due to ethical restrictions on altering treatment for depressed patients. This limitation underscores the difficulty in disentangling the genuine pharmacological effects of SSRIs from placebo responses often seen in antidepressant studies. As a result, distinguishing whether observed benefits stem from SSRIs specifically or merely arise from patients’ expectations remains a contentious issue.
Moreover, while the improvements in depression among patients are noteworthy, numerous studies have thrown SSRIs’ efficacy into doubt, suggesting they might not outperform placebo treatments for many individuals. The longstanding theory of serotonin deficiency in depression has also been scrutinized, fueling ongoing debates within the psychiatric community.
The necessity for further research cannot be overstated. As researchers and clinicians work to comprehend the full spectrum of SSRIs’ effects, the need to explore alternative pharmacological strategies becomes increasingly paramount for advancing precision psychiatry. Discovering targeted treatments could lead to improved outcomes, particularly for cognitive impairments commonly associated with mood disorders.
It is crucial to recognize that these findings, while promising, represent just a preliminary step in addressing a multifaceted issue. Mental health treatments inherently require careful navigation; none should cease SSRI usage without thorough discussion with a healthcare provider due to the potential for adverse effects. As the field of psychiatry progresses, understanding the mechanisms of action of SSRIs and exploring groundbreaking therapeutic avenues will play a vital role in enhancing patient care.
As anxiety and depression continue to grip millions globally, the quest for clarity around SSRIs not only holds patients’ well-being in its balance but may also pave the way for innovative therapies that address both cognitive and emotional challenges in mental health. The ongoing journey of research is one that is both critical and compelling, hinting that the ties between psychology, neurochemistry, and pharmacology are more nuanced than previously understood.

Leave a Reply