In the evolving landscape of Alzheimer’s disease research, a beacon of hope flickers with the recent trials suggesting that methods aimed at slowing disease progression could effectively delay its onset in at-risk individuals. This groundbreaking news, heralded by Randall J. Bateman, a neurologist at Washington University, ignites a flame of optimism among families grappling with the potential loss of loved ones to this cruel illness. The implication is staggering; if future advancements can delay Alzheimer’s disease for even a fraction of the millions poised to inherit its burdens, it transforms the narrative from one of despair to one of proactive empowerment.
The recent study focused on a mere 73 participants, all carrying mutations tied to Dominantly Inherited Alzheimer’s. While this genetic variant represents merely 1% of Alzheimer’s cases, those afflicted have an unsettling inevitability about their fate—by their 50s, they are almost guaranteed to develop symptoms. In the face of such overwhelming odds, it becomes abundantly clear that this research is not just another drop in an ocean of scientific inquiry; it is a critical lifeline for those who find themselves on the brink of generational trauma.
A Cautious Approach to Treatment
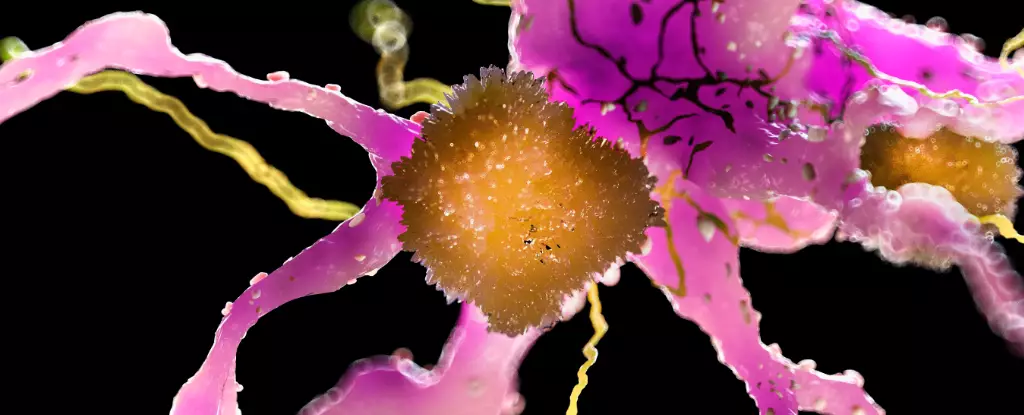
The trial’s design reinforces the challenges often faced in clinical settings, particularly with methods that leverage immunotherapy through antibody combinations. While hope blossomed from initial findings regarding gantenerumab—a drug that showed promise in altering the pathology of Alzheimer’s—the road has not been devoid of obstacles. Previous phase 3 trials failed to show movement in cognitive symptoms, reflective of a broader issue in Alzheimer’s research; the disconnect between biological markers and clinical outcomes often leaves patients standing in the limbo between science and suffering.
Nevertheless, hope was reignited when researchers identified that higher doses of gantenerumab could yield better results. Participants who continued in the trial displayed a shocking statistical decline in their risk of cognitive deterioration, cutting their chances of developing symptoms by half. Yet, as we celebrate such victories, it is crucial to temper our enthusiasm with a prudent awareness of the risks associated with these treatments. Gantenerumab and similar therapies have been linked to adverse side effects, including the ominous specter of microbleeds in the brain. Such complications inherently complicate patient treatment plans and raise ethical questions surrounding the management of risk versus reward in clinical settings.
A Glimpse of the Future
This juxtaposition of hope and caution leads to a broader dialogue about the nature of Alzheimer’s research and the potential evolution of preventive measures. If researchers can secure that “delay” rather than an outright cure, it may still represent a victory worth celebrating. The specter of neurodegeneration hangs heavily over the lives of countless families, and for some, the prospect of an extended period of healthy cognition is life-altering. Bateman’s assertions that delaying the onset of symptoms could lead to “more years of healthy life” resonate deeply with anyone who has witnessed the brutal progression of Alzheimer’s.
Moreover, the prospect of delaying Alzheimer’s symptoms introduces the tantalizing potential for improved quality of life, not just for those genetically marked for decline but also for the caregivers and families intertwined in their journeys. The national conversation about aging and neurodegenerative diseases is ripe for transformation, underscoring the urgent need for innovative public policies that address not only the needs of those already afflicted but also prioritize research funding and accessibility to emerging therapies.
Hope Amid Uncertainty
While it’s easy to view this new research through a lens of cautious optimism, the sketch of Alzheimer’s treatment approaches in the future remains incomplete. With several leading next-generation treatments poised to enter the fray, the conversation is shifting toward a focus on preemptive measures rather than solely post-symptomatic care. This pivot could realign our approach to health care, transforming the methodology from reactionary to preventative.
Still, as we stand on the precipice of potential breakthroughs, we must grapple with the harsh reality that this journey is fraught with risk, uncertainty, and ethical dilemmas. The stakes are undeniably high, yet the torch of hope continues to burn brightly for those determined to defend their cognitive futures against one of humanity’s most formidable adversaries.

Leave a Reply