The recent advancements in Alzheimer’s treatment, particularly with drugs like lecanemab, herald promise for millions struggling with cognitive decline. However, what appears as a beacon of hope may be a selective lifeline that fails to adequately assist the majority of sufferers: women. Clinical trials indicate that while lecanemab can slow cognitive decline by as much as 27 percent in general, a disconcerting disparity arises when it comes to sex-based responses. For men, the drug’s efficacy showcases a staggering 43 percent reduction in cognitive deterioration, contrasted sharply by a mere 12 percent for women. This raises both ethical and scientific questions about representation in clinical trials and drug effectiveness, warranting a closer examination of how these imbalances affect overall healthcare.
The Hidden Risks of Sex-Based Differences
A comprehensive analysis points to a 31 percent gap in drug response between sexes, a figure that cannot be ignored. While some may argue that these statistics are insignificant or merely result from variability in trial conditions, the implications run far deeper. Neuroscientist Daniel Andrews and his colleagues reveal that the existing biological differences in brain function and aging cannot fully explain the observed disparity. This notion casts a shadow on the legitimacy of lecanemab and indeed, on the larger quest for effective Alzheimer’s treatments. With two-thirds of all Alzheimer’s patients being women, ignoring their unique physiological and psychological needs represents not just a missed opportunity for clinical success, but a profound injustice as well.
Clinical Trials: A Deficit in Inclusivity
As the debate continues, one must confront the uncomfortable truth hiding in the shadows of medical research: there has been a conspicuous lack of attention to sex-based differences in clinical trial design. Neuroscientists lament the historical oversight, citing that recruitment practices have often neglected to strategically ensure a representative sample across gender lines. Such negligence risks compounding the already omnipresent biases in medical outcomes. Critically, scrutiny has emerged towards the common practice of presenting subgroup data in complex formats like forest plots without robust statistical backing for gender comparisons. This lack of clarification further muddies the waters when we attempt to glean actionable insights from trial results.
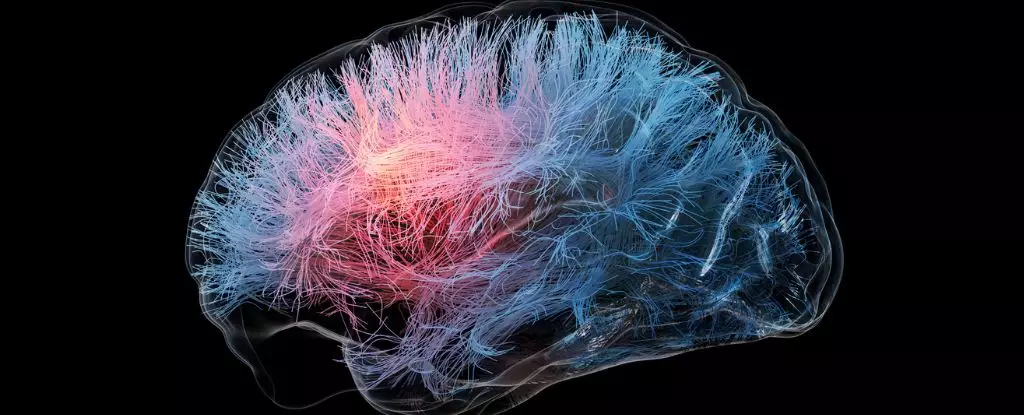
Investigating the Brain: A Complex Puzzle
The mechanics of lecanemab reveal an arrow aimed at amyloid plaques, which have long been deemed central to the development of Alzheimer’s. Yet, as research deepens, the narrative has shifted: amyloid plaques may not simply be the enemy but a marker among many in a multifaceted disease landscape. In fact, some studies suggest a third of Alzheimer’s patients exhibit no such plaques upon postmortem examination. This highlights a dire need for researchers to disentangle biological complexities, especially when considering how sex hormones might influence the formation and removal of these plaques. It compels one to ask: are we treating the right disease at all?
Pioneering a New Frontier of Research
The consequences of neglecting sex differences extend far beyond medical treatment; they ripple into individual lives. The voices advocating for change in how trials are conducted stress the urgent need for drug developers to collaborate and share data that can illuminate underlying mechanisms. This necessity is echoed by an international response that reveals an alarming 95 percent of neuroscience studies ignore sex considerations, leading to a systemic neglect that could severely impede our understanding of Alzheimer’s and other cognitive disorders.
The imbalance permeates not just the learning and understanding of diseases but the wellness outcomes for millions who live in the shadows of these diseases. Moving forward, it’s vital that neurologists and pharmaceutical companies prioritize gender diversity in research settings. The implications are profound; an equitable approach could lead to treatments that save lives and enhance the quality of life for all patients, regardless of their sex.
A Call to Action
The grand paradox thus becomes clear: as we celebrate groundbreaking medications like lecanemab, we must simultaneously hold them accountable to the full spectrum of potential beneficiaries. Ignoring the significant potential variance in treatment efficacy based on sex not only compromises scientific integrity but jeopardizes the health of millions of women facing Alzheimer’s. As we advocate for a more equitable medical landscape, one where treatments genuinely reflect the complexities of both male and female biologies, we must strive for inclusivity in clinical trials. Only then can we hope to usher in a new era of neuroscience informed by a more holistic, nuanced understanding of our diverse populations.

Leave a Reply